Project in Progress :
Macrolides and airway remodeling reversibility
Dr Sophie Mainguy-Seers
Asthma is a chronic disease of the airways affecting 235 millions of individuals according to the World Health Organization and touches approximately 8% of Canadians. While a minority of patients are severely affected (≈5-10%), their quality of life is markedly impaired and they require high healthcare costs.1
Particularly, a sub-group of severe asthmatics with neutrophilic airway inflammation are poorly responsive to current therap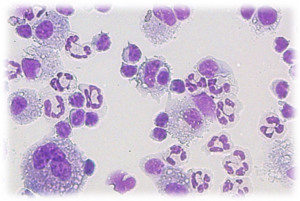 y and lung dysfunction and neutrophils persist in the respiratory tract despite medication. Airway neutrophilia has been associated with the progression of the disease and the presence of structural alterations of the airways (‘’remodeling’’).2
y and lung dysfunction and neutrophils persist in the respiratory tract despite medication. Airway neutrophilia has been associated with the progression of the disease and the presence of structural alterations of the airways (‘’remodeling’’).2
The prolonged use of macrolides have been shown to improve the quality of life and to reduce the frequency of exacerbations in asthmatics.3Those antibiotics possess immunomodulatory properties and appear especially useful in respiratory diseases mediated by neutrophilic inflammation.4Interestingly, studies in experimental model of asthma (rodents) suggest that this class of medication might improve airway remodeling.5
Therefore, the goal of this project is to elucidate if macrolide treatment can reduce bronchial remodeling more than what is obtained with current therapy (inhaled corticosteroid) by studying the model of equine asthma.
Severe equine asthma is similar to the human condition, as both diseases are characterized by respiratory obstruction, mucus accumulation in the airways and bronchial inflammation (neutrophilic in horses) and remodeling. In asthma, the structural changes mainly occur in the small airways, however those bronchi are not easily accessible in asthmatic individuals. On the contrary, they can be harvested sequentially in horses due to the large size of their lungs and the possibility to do standing thoracoscopic surgery, allowing the study of bronchial remodeling.
In order to achieve the objectives of this research project, multiple aspects will be studied, including the effects of macrolide on lung function, on pulmonary inflammation, on genic expression of several tissue samples and on airway remodeling of asthmatic horses.
By studying the therapeutic potential of macrolides in asthma, we aim to clarify if the use of these antibiotics is ethically justified. Indeed, they are often administered for the treatment of severe human asthmatics despite concerns on the development of antimicrobial resistance. Therefore, if this study shows a clinical usefulness to their administration, it could fasten the development of macrolides that lack antimicrobial effects.
- FitzGerald JM et al. Recognition and management of severe asthma: A Canadian Thoracic Society position statement. Canadian Journal of Respiratory, Critical Care, and Sleep Medicine 2017;1:199-221
- Shaw DE et al. Association between neutrophilic airway inflammation and airflow limitation in adults with asthma. Chest 2007;132:1871-1875.
- Gibson PG et al. Effect of azithromycin on asthma exacerbations and quality of life in adults with persistent uncontrolled asthma (AMAZES): a randomised, double-blind, placebo-controlled trial. Lancet 2017;390:659-668.
- Kanoh S, Rubin BK. Mechanisms of action and clinical application of macrolides as immunomodulatory medications. Clin Microbiol Rev 2010;23:590-615.
- Kang JY et al. Long-term azithromycin ameliorates not only airway inflammation but also remodeling in a murine model of chronic asthma. Pulm Pharmacol Ther 2016;36:37-45.
Development of a protocol for the recellularization of a decellularized equine bronchial matrix
Dr Selma Ben Hamouda
Severe asthma is a chronic respiratory syndrome associated with an alteration in airway smooth muscle mass and in the composition of the extracellular matrix. The interactions occurring between the extracellular matrix and the bronchial smooth muscle cells contribute to this remodeling and to the limited response to therapy. Three-dimensional matrices allow to capture the complex cellular response of airway smooth muscle cells to the bronchial extracellular matrix. We established a protocol to decellularize equine bronchi and then recellularize them with primary airway smooth muscle cells. Results showed that smooth muscle cells migrated into the decellularized smooth muscle layer suggesting that beyond the mechanistic factors, the scaffold induced a chemotactic effect on these cells.
Study of bronchial extracellular matrix influence on airway smooth muscle cells in asthma using an equine 3D bronchial model
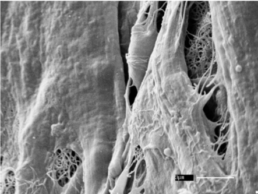
Dr Selma Ben Hamouda
The interactions occurring between the bronchial extracellular matrix (ECM) and the smooth muscle cells (SMC) in asthma contribute to the airway remodeling and to the limited therapeutic response. Three-dimensional cell culture offers the possibility to study the ECM-SMC interactions in an almost natural environment. Using the protocol cited above, we aimed to mix and match different control and asthmatic ECM with different control and asthmatic SMC. We then used the resulting tissues to study the influence of the ECM on the SMC and vice versa. To do so, we used histology, scan electron microscopy on tissue surface and cross sections and next gene sequencing. Work still in progress.
Studies of Molecular Pathways Associated with Insensitivity to Neutrophil Corticosteroids in Equine Asthma
Sheila Pourali Dogaheh
Our hypothesis is that bio-activators stimulated by the microenvironment in airway inflammation may contribute to insensitivity of neutrophils to corticosteroids in asthmatic horses.
Neutrophil function will be studied by comparing viability, apoptosis, pro-inflammatory gene and protein expression of neutrophils under culture conditions simulating hypoxemia and oxidative stress.
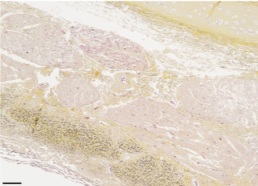
Quantification of angiogenesis in equine asthma
Dr Esther Millares Ramirez
Equine asthma is a chronic disease of the airways that is characterized by inflammation and structural changes of the airway. This disease is not 100% reversible with treatment. Multiple causes of the structural changes have been studied, however angiogenesis (formation of new vessels) have never been studied before. Our hypothesis is that angiogenesis is increased in horses in exacerbation in comparison with control horses. And that demonstrating that, we could help improve the treatment of horses with this disease.
Systemic effects of intra-articular corticosteroids in asthmatic horses
Dr Esther Millares Ramirez
Intra-articular (IA) administration of corticosteroids is performed routinely in equine practice. Horses with poor performance issues but without any orthopedic problems could improve with these treatments. Recent work from our laboratory showed an improvement of the lung function of severe asthmatic after IA triamcinolone acetonide (TA). We therefore hypothesized that IA methylprednisolone acetate (MPA), another commonly used corticosteroids, would also decrease the airway obstruction in severe asthmatic horses.
Angiogenesis: response to treatment with corticosteroids
Dr Esther Millares Ramirez
On previous studies we demonstrated the presence of angiogenesis in central airways of asthmatic horses. The objective of our study is to evaluate the angiogenic response to treatment with corticosteroids. Our hypothesis is that angiogenesis will mildly decrease with treatment.
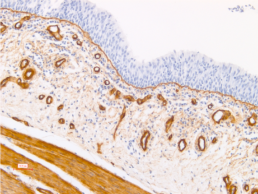
Study of smooth muscle remodeling in moderate asthmatic horses

Florence Dupuis-Dowd
The inflammation occurring in lower respiratory tracts of asthmatic horses induces remodelling of the airways. Increased mass of airways smooth muscles(ASM), increased ASM myocytes turn over, and overexpression of the (+) Insert isoform of myosin are main features that have been previously described in severe asthmatic horses by our laboratory. Although muscle phenotype of severe asthmatic horses has been well defined, phenotype of mild and moderate subjects needs further characterisation. We hypothesize that, when present, phenotypic changes of ASM of mild and moderate asthmatic subjects could lead to the development of the severe from of the disease. By performing immunohistochemistry(IHC) on paraffine embedded endobronchial biopsies(EBB) and qPCR on other EBB of the same horses, we aim to define changes of ASM occurring in early stages of equine asthma. The identification of these changes, and their characterisation, could lead to new biomarkers to diagnose earlier, and eventually prevent, equine asthma.